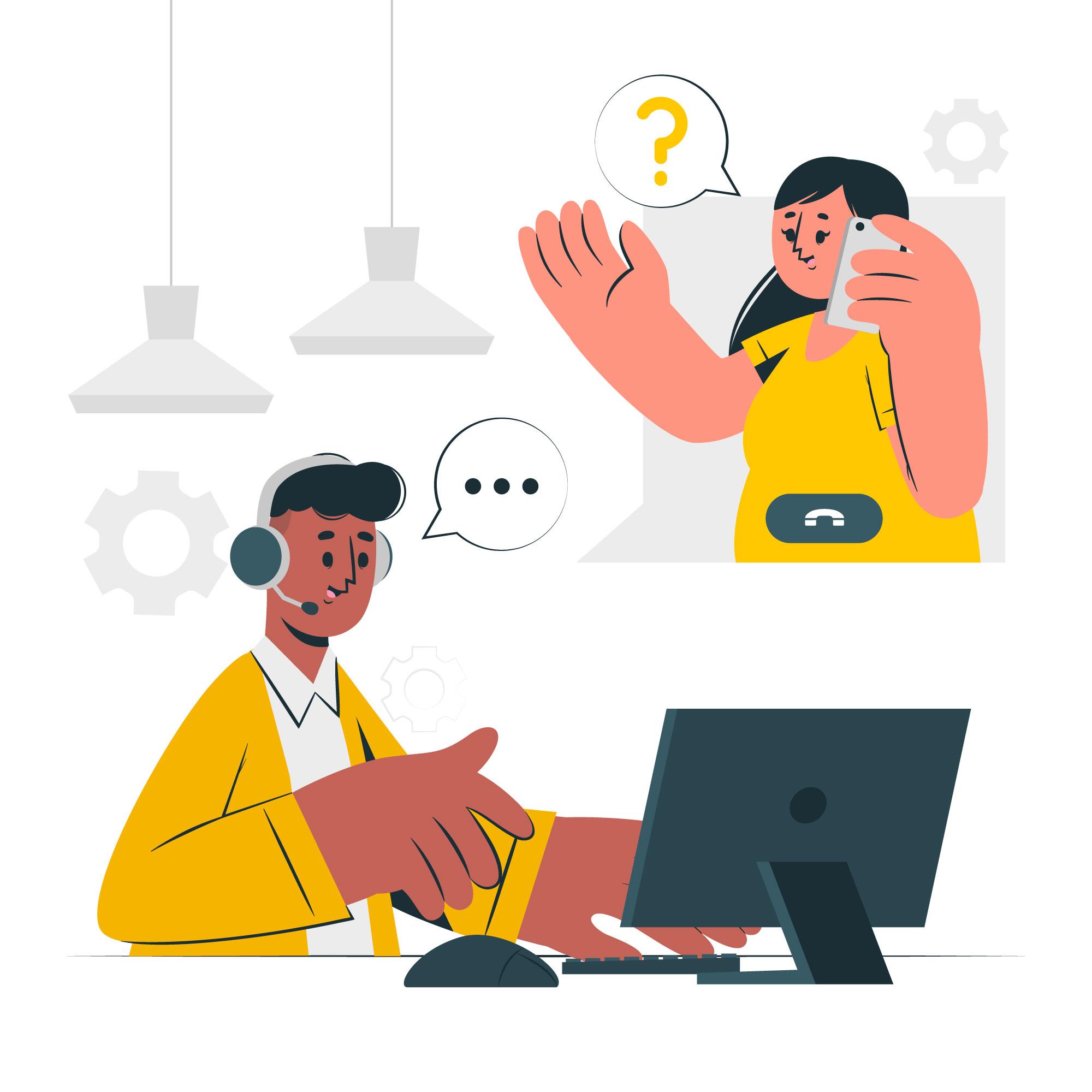
Expert Plan Guidance
Get clear explanations of your healthcare plan, benefits, and coverage options.
Assistance in understanding key terms like premiums, deductibles, out-of-pocket maximums, and coinsurance.
Help with reviewing your benefits to ensure you’re fully aware of what’s available to you.